Key Points
- AI can help healthcare leaders solve persistent challenges, but layering on top of legacy systems creates technical debt that slows modernization.
- Khalid Turk, Chief Healthcare Information Officer at Santa Clara County, told CIO News how adding AI "wrappers" on existing infrastructure can introduce risk.
- Governance and human-in-the-loop requirements will determine which AI debts leaders accept, he said, with patient trust setting the ceiling for autonomy.
For healthcare leaders, AI promises to solve many of the industry’s most persistent challenges: physician burnout, operational inefficiencies, and declining revenue. Yet in the rush to adopt it, many are discovering a troubling side effect. Each new AI layer adds fragility on top of legacy systems. Now, the resulting technical debt threatens to slow the very transformation this technology promises.
To understand the actual cost of AI in healthcare, we spoke with Khalid Turk, Chief Healthcare Information Technology Officer for the County of Santa Clara, one of the largest public health systems in America. Here, he leads a team of over 250 professionals, managing IT operations across four hospitals and more than 20 clinics serving 14,000 users. Before becoming a CHIO, Turk was a software engineer writing the very code that holds his hospitals together. His experience with large-scale EMR integrations and digital transformations enables Turk to see AI as both a strategist and an engineer.
An inevitable debt: The very speed of AI's evolution is the source of this new debt, Turk explained. When technology advances at an unprecedented pace, today's cutting-edge solution becomes tomorrow's legacy problem, seemingly overnight. "With AI, we are introducing technical debt for ourselves for the future. Technical debt is the long-term cost of choosing an easy solution now instead of using a better approach that would take longer. Because AI is evolving so fast, many of the systems we're implementing today won't be able to scale or transform readily tomorrow."
The decision to incur this debt is not arbitrary, Turk continued. Instead, it's a direct response to one of three critical business pressures. "The drive to adopt AI isn't random. Is your goal to increase revenue? Is it to improve efficiency and reduce provider 'pajama time'? Or is it to create better patient engagement? Your AI strategy will be completely different depending on which of those one, two, or all three problems you're trying to solve."
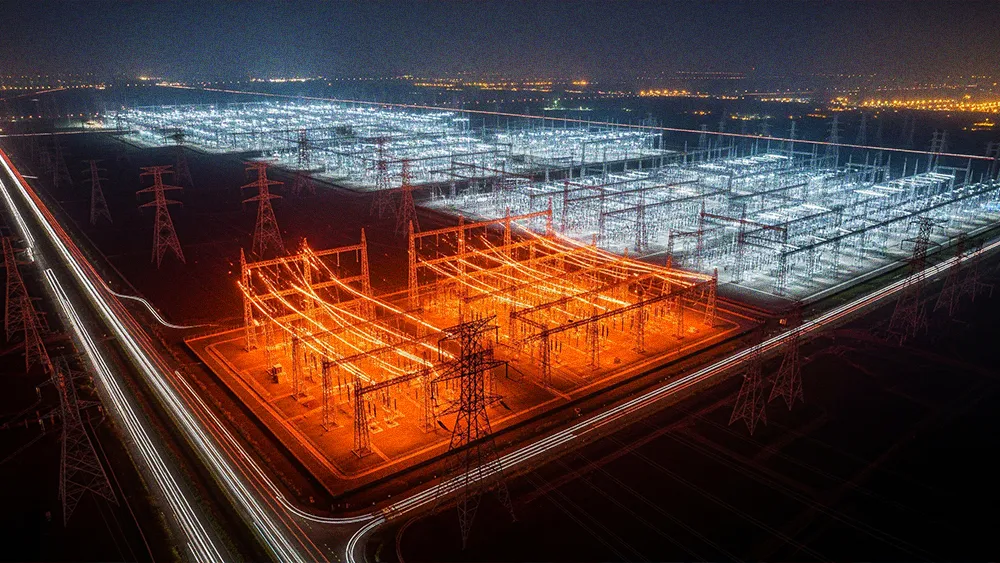
Wrappers on wrappers: Often, these solutions are just "wrapper" technologies layered on top of aging, inflexible systems, Turk cautioned. The result is a form of "institutional debt" that emerges through vendor lock-in. For example, he pointed to the market’s dominant EMRs. Because their foundational client-server designs are ill-suited for modern AI, vendors are forced to bolt on solutions rather than integrating them natively, he said. "Most AI in the EMR sphere today is just a wrapper on existing technology. The core systems are often built on older architectures, which do not lend themselves to AI. To compensate, they build a cloud service. An API call goes from the on-premise system to the cloud and back. It works, but it's not a native solution. It's a layer bolted onto a legacy foundation."
The sunk-cost anchor: Institutional debt makes it especially challenging for large health systems to switch to newer, AI-native systems, Turk said. "Think of it like a $10 million house. Even if you don't like it, the cost to change it is enormous. Over the past 12 years, we've invested nearly $300 million in our system. To let go of that investment, plus all the customization, user training, and familiarity we've built, just to start over with a new product and go through another five-year cycle to make it mature? That is a monumental decision for any organization to make."

Next, he described the challenge for CIOs with a simple but powerful analogy. "When you look at the AI market today, it's not like there's one Costco where you can go and buy everything you need. Instead, you have to visit the entire mall, going to dozens of different stores, just to find the products you can use. That fragmentation is a massive challenge for any CIO trying to build a coherent system."
In a surprising twist, however, Turk said AI could also be the cure for one of healthcare’s oldest forms of technical debt. After decades of struggling with brittle, custom-coded interfaces that take weeks to build, he sees a surprising path forward. More specifically, his personal experience tinkering with LLMs revealed their unexpected power to solve long-standing integration challenges.
Poison and antidote: "I was surprised at how capable even non-specialized LLMs are at HL7 transformation and interpretation. Imagine an AI agent that can manage these interfaces automatically. When a system is upgraded and a data field moves, the agent sees it and adjusts accordingly, no programmer required. We're not there yet, but AI could solve one of the most painful, time-consuming problems in healthcare IT."
Ultimately, the biggest hurdle for AI in healthcare is not technical or financial, Turk concluded. It's cultural and ethical. The irreversible nature of clinical failure restricts the pace of autonomous AI adoption in healthcare. For him, that raises the ethical bar considerably. "The fundamental question is: will healthcare ever be ready for a 'human out of the loop' model? The stakes are simply too high. A billion-dollar loss in finance can be recovered. A single human life cannot. That risk is what will always delay, if not entirely prevent, us from fully adopting autonomous agentic AI, no matter how advanced it becomes."
The question for healthcare leaders is not if they will adopt AI, Turk said. They will. The more important decision is which technical, financial, and cultural debts they are willing to take on. Nonetheless, every decision must be measured against the core principle of medicine, he continued. Instead of ROI, the final test for any AI tool is its impact on a far more valuable currency. "It comes down to trust. Patients open up to doctors because they trust them. Trust is the currency of the healthcare system, and AI can easily erode it. So, when you introduce any technology into the health system, you have to ask, 'Am I going to breach that trust?' If the answer is yes, then no matter how good the technology is, it doesn't belong here."
.svg)